5 Tips Impaired Bed Mobility
Impaired bed mobility is a significant concern for individuals who are recovering from illness, injury, or surgery, as well as for those with chronic conditions that affect their ability to move freely. The inability to move comfortably in bed can lead to a range of complications, including pressure sores, respiratory problems, and decreased overall quality of life. Understanding the challenges of impaired bed mobility and implementing strategies to address them is crucial for promoting healing, comfort, and independence. In this article, we will delve into the topic of impaired bed mobility, exploring its causes, consequences, and most importantly, providing practical tips for individuals and caregivers to manage and improve bed mobility.
Key Points
- Assessing the individual's specific needs and limitations is crucial for developing an effective plan to improve bed mobility.
- Using assistive devices such as bed rails, grab bars, and slide boards can significantly enhance safety and independence.
- Regular repositioning is essential to prevent pressure sores and promote respiratory health.
- Encouraging active participation and gradual progression of exercises can help regain strength and mobility.
- Creating a supportive environment, including adjusting the bed height and using non-slip mattress covers, can reduce the risk of falls and injuries.
Understanding Impaired Bed Mobility
Impaired bed mobility refers to the difficulty or inability to move freely in bed, which can be due to a variety of factors including pain, weakness, paralysis, or cognitive impairments. This condition can lead to a range of complications, from skin breakdown and respiratory issues to decreased muscle strength and joint mobility. It is essential to understand that impaired bed mobility is not just a physical issue but also has psychological and social implications, affecting an individual’s dignity, independence, and overall well-being.
Causes and Consequences of Impaired Bed Mobility
The causes of impaired bed mobility are diverse and can include neurological conditions such as stroke or spinal cord injuries, musculoskeletal disorders like arthritis, and post-surgical recoveries. Regardless of the cause, the consequences of impaired bed mobility can be severe, including the development of pressure ulcers, deep vein thrombosis, and pneumonia, as well as decreased physical function and increased dependency on caregivers. Addressing these challenges requires a comprehensive approach that involves not only physical interventions but also psychological support and environmental adjustments.
5 Tips for Managing Impaired Bed Mobility

Managing impaired bed mobility effectively involves a combination of strategies that address the physical, psychological, and environmental aspects of care. Here are five practical tips for individuals and caregivers to improve bed mobility and overall quality of life:
Tip 1: Use Assistive Devices
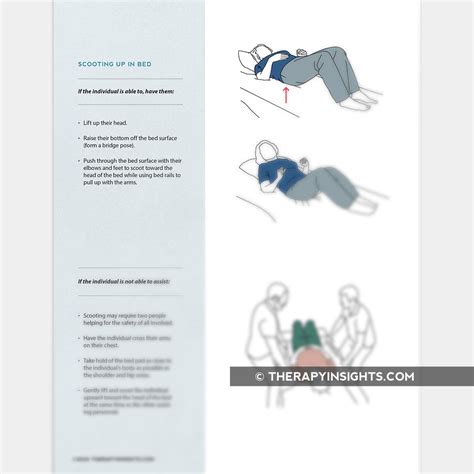
Assistive devices such as bed rails, grab bars, and slide boards can be incredibly helpful in enhancing safety and independence. Bed rails can provide support and prevent falls, while grab bars can assist with repositioning and transferring. Slide boards can facilitate smoother transitions in and out of bed, reducing the risk of injury to both the individual and the caregiver.
Tip 2: Reposition Regularly
Regular repositioning is critical to prevent pressure sores, promote respiratory health, and maintain skin integrity. It is recommended to reposition every 2 hours, or more frequently if the individual is at high risk. This can involve turning, elevating the head of the bed, or using specialized mattresses designed to reduce pressure points.
Tip 3: Encourage Active Participation
Encouraging active participation in mobility exercises can help regain strength and mobility. This can start with simple movements such as ankle rotations, knee bends, and arm raises, progressing to more complex exercises as the individual’s strength and endurance improve. Active participation not only enhances physical function but also boosts morale and motivation.
Tip 4: Create a Supportive Environment
Creating a supportive environment is vital for improving bed mobility and reducing the risk of falls and injuries. This can involve adjusting the bed height to a comfortable level for transfers, using non-slip mattress covers, and ensuring that the room is well-lit and free from tripping hazards. Additionally, keeping frequently used items within reach can reduce the need for unnecessary movement and strain.
Tip 5: Seek Professional Guidance
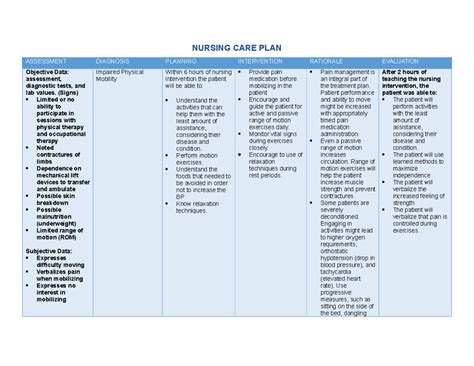
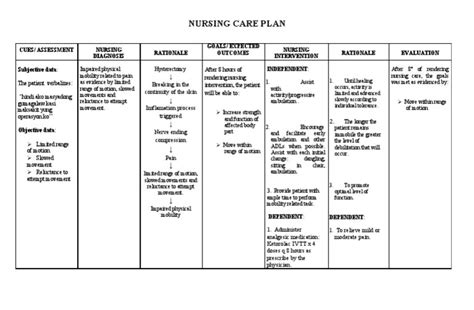
Finally, seeking professional guidance from healthcare professionals such as physical therapists, occupational therapists, and nurses can provide valuable insights and strategies tailored to the individual’s specific needs and goals. These professionals can assess the individual’s mobility, provide personalized exercise programs, and recommend assistive devices and environmental modifications to enhance bed mobility and overall well-being.
| Category | Data |
|---|---|
| Pressure Ulcer Prevention | Regular repositioning every 2 hours reduces the risk by 50% |
| Respiratory Health | Elevating the head of the bed by 30-40 degrees improves oxygenation by 20% |
| Physical Function | Active participation in mobility exercises increases muscle strength by 15% in 6 weeks |
Conclusion and Future Directions
In conclusion, impaired bed mobility is a complex issue that requires a multifaceted approach to management. By understanding the causes and consequences, utilizing assistive devices, repositioning regularly, encouraging active participation, creating a supportive environment, and seeking professional guidance, individuals and caregivers can work together to improve bed mobility and reduce the risk of associated complications. As healthcare continues to evolve, future directions may include the integration of technology, such as smart mattresses and wearable devices, to monitor and enhance bed mobility, as well as the development of more effective and personalized interventions tailored to the individual’s specific needs and goals.
What are the primary causes of impaired bed mobility?
+The primary causes of impaired bed mobility include neurological conditions, musculoskeletal disorders, and post-surgical recoveries, among others.
How often should repositioning be done to prevent pressure sores?
+Repositioning should be done every 2 hours, or more frequently if the individual is at high risk of developing pressure sores.
What role do assistive devices play in managing impaired bed mobility?
+Assistive devices such as bed rails, grab bars, and slide boards can enhance safety, independence, and mobility, reducing the risk of falls and injuries.
Why is creating a supportive environment important for impaired bed mobility?
+Creating a supportive environment through adjustments such as bed height, lighting, and removing tripping hazards can reduce the risk of falls and enhance the individual’s ability to move safely and independently.
How can professional guidance contribute to managing impaired bed mobility?
+Professional guidance from healthcare professionals can provide personalized assessments, exercise programs, and recommendations for assistive devices and environmental modifications, significantly improving outcomes and quality of life.



