Impaired Mobility Nursing Care Plan
Impaired mobility is a common concern in nursing care, affecting patients across various settings, from acute care hospitals to community and home care environments. It refers to the limitation or inability to move or walk, which can be caused by a wide range of factors including but not limited to neurological conditions, musculoskeletal disorders, cardiovascular diseases, and aging. The goal of a nursing care plan for impaired mobility is to maximize the patient's mobility and function, preventing complications associated with immobility, and enhancing overall quality of life.
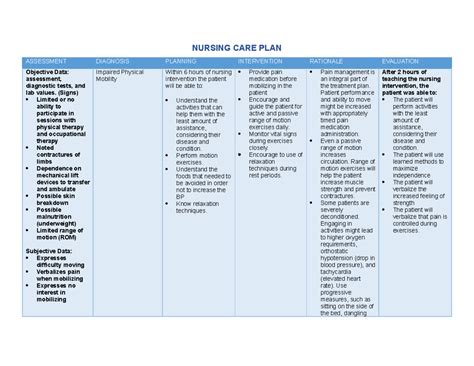
Assessment and Diagnosis
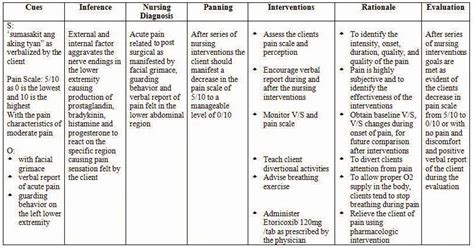
The first step in developing a care plan for a patient with impaired mobility is a comprehensive assessment. This involves evaluating the patient’s current mobility status, medical history, and the underlying cause of the impaired mobility. The assessment should include a physical examination, review of the patient’s medical history, and possibly, the use of standardized assessment tools to measure mobility and functional ability. Based on the assessment findings, the nurse can formulate a nursing diagnosis. A common nursing diagnosis for patients with impaired mobility is “Impaired Physical Mobility” related to weakness, pain, or musculoskeletal impairment.
Risk Factors and Complications
Patients with impaired mobility are at risk for several complications, including pressure ulcers, deep vein thrombosis, pneumonia, urinary tract infections, and contractures. Understanding these risk factors is crucial for the development of an effective care plan. The nurse should identify specific risk factors for each patient and incorporate strategies to mitigate these risks into the care plan.
| Complication | Prevention Strategy |
|---|---|
| Pressure Ulcers | Regular repositioning, use of pressure-redistributing mattresses, and skin inspection |
| Deep Vein Thrombosis | Use of anti-embolic stockings, pneumatic compression devices, and mobilization as tolerated |
| Pneumonia | Encouraging deep breathing exercises, coughing, and early mobilization |
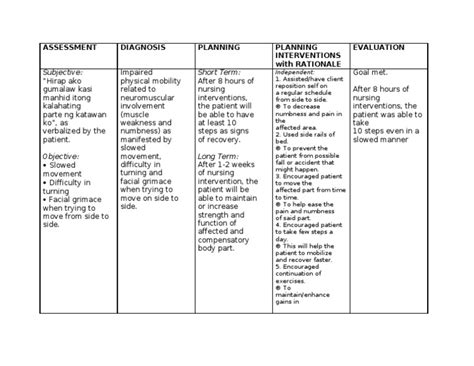
Interventions and Implementation
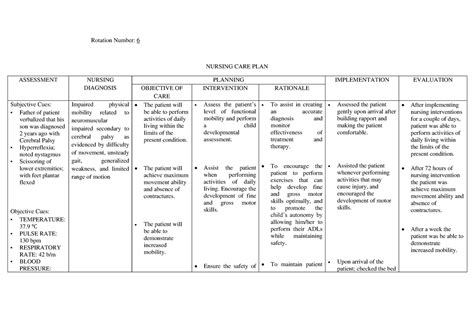
The care plan for a patient with impaired mobility should include a range of interventions tailored to the patient’s specific needs and goals. These may include physical therapy to improve strength and mobility, pain management to facilitate movement, and education on safe transfer techniques to prevent injury. The nurse should work collaboratively with other healthcare professionals, such as physical therapists and occupational therapists, to develop and implement the care plan.
Patient Education
Patient education is a critical component of the care plan, empowering patients and their families to manage impaired mobility effectively. Education should cover topics such as proper body positioning, techniques for safe transfer, and the importance of regular exercise and mobility. The nurse should also provide guidance on how to prevent complications and when to seek medical help.
Key Points
- Comprehensive assessment is the foundation of an effective care plan for impaired mobility.
- Early mobilization and regular exercise can significantly improve mobility and prevent complications.
- Patient education and family involvement are crucial for long-term management of impaired mobility.
- Collaboration with other healthcare professionals enhances the effectiveness of the care plan.
- Continuous monitoring and adjustment of the care plan are necessary to address changing patient needs.
Evaluation and Revision
Evaluation of the care plan’s effectiveness is ongoing, with regular assessments of the patient’s mobility and functional ability. The nurse should revise the care plan as necessary based on the patient’s progress, new concerns, or changes in the patient’s condition. This may involve adjusting interventions, setting new goals, or incorporating additional strategies to address emerging needs.
Outcome Measurement
Measuring outcomes is essential to determine the effectiveness of the care plan. This can be achieved through the use of standardized tools and metrics that assess mobility, functional status, and the presence of complications. By regularly evaluating outcomes, the nurse can refine the care plan to better meet the patient’s needs and improve overall care quality.
What are the primary goals of a nursing care plan for impaired mobility?
+The primary goals are to maximize the patient's mobility and function, prevent complications associated with immobility, and enhance overall quality of life.
How often should a patient with impaired mobility be repositioned?
+Patients should be repositioned at least every 2 hours, or more frequently as needed, to prevent pressure ulcers and promote comfort.
What role does patient education play in the management of impaired mobility?
+Patient education empowers patients and their families to manage impaired mobility effectively, covering topics such as safe transfer techniques, exercise, and complication prevention.
In conclusion, impaired mobility requires a comprehensive and tailored nursing care plan that addresses the patient’s specific needs and goals. Through early assessment, collaborative care planning, patient education, and ongoing evaluation, nurses can play a critical role in improving mobility, preventing complications, and enhancing the quality of life for patients with impaired mobility.